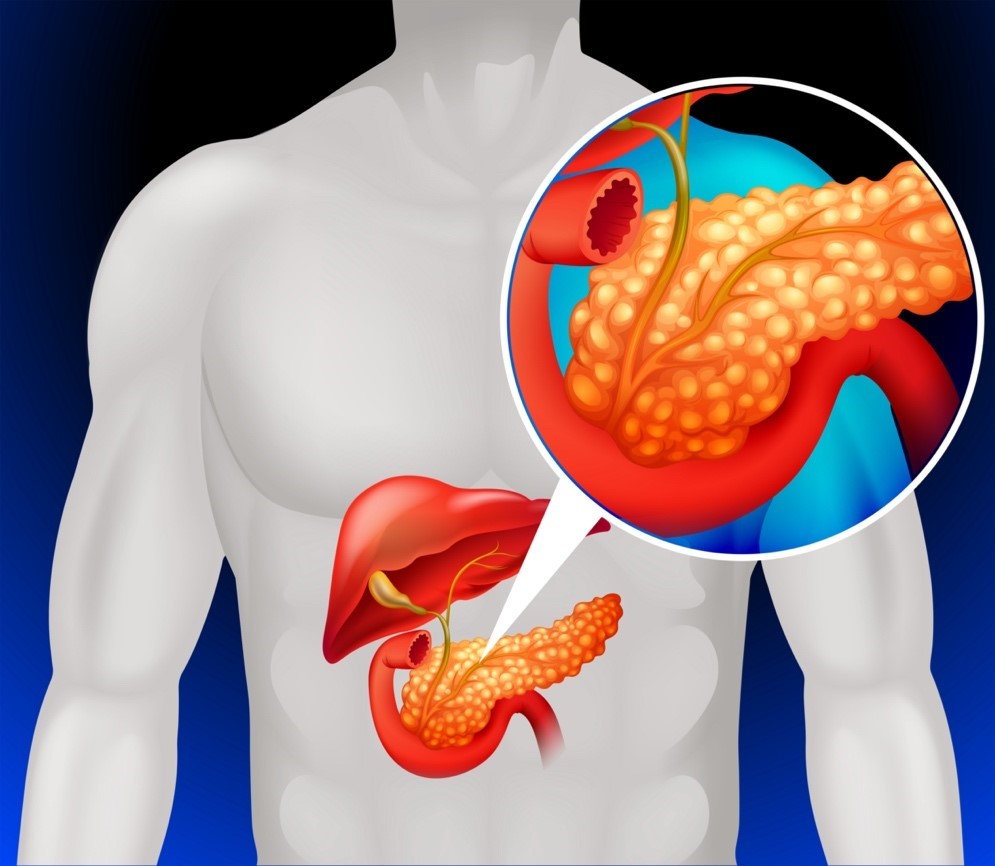
Pancreas is a long, flat gland tucked away in the abdomen, which plays a significant role in the digestion of food and regulation of blood sugar. When it becomes inflamed, it causes mild discomfort to severe, life-threatening symptoms.
Pancreatitis is an inflammatory condition of the pancreas that disrupts its normal functioning. Pancreatitis can be acute- appears suddenly and lasts for a short duration. Chronic pancreatitis is a long-term condition, in which the pancreas get worse with time.
In this patient education blog, we will explore more about the symptoms, causes, diagnosis, treatment strategies of pancreatitis.
Symptoms
The symptoms of pancreatitis can vary depending on whether the condition is acute or chronic. Here are some common symptoms for both:
Acute Pancreatitis:
- Severe upper abdominal pain, often radiating to the back
- Pain that intensifies after eating
- Abdominal pain that feels worse when lying down
- Nausea and vomiting
- Fever
- Rapid pulse
- Swollen and tender abdomen
Chronic Pancreatitis:
- Upper abdominal pain
- Unintentional weight loss
- Oily, smelly stools (steatorrhea)
- Diarrhea
- Nausea and vomiting
What causes pancreatitis?
- Heavy alcohol use
- Certain medicines
- High triglyceride levels in the blood
- High calcium levels in the blood
- Genetic predispositions
- Pancreas cancer
- Injuries from trauma/surgery
Complications Associated with pancreatitis
Most of the acute pancreatitis' cases improve on its own. However, few cases are severe, resulting in:
- Infection
- Bleeding
- Pancreatic Cancer
- Malnutrition
- Diabetes
- Breathing Problems
- Kidney Failure
- Pancreatic Necrosis
- Organ Failure
How to diagnose pancreatitis?
Diagnosing pancreatitis involves a combination of clinical evaluation, blood tests to check elevated enzyme levels, and imaging studies like CT scans or MRIs. These tests are essential to confirm the diagnosis and assess the severity of the condition.
Treatment
Managing pancreatitis often requires a multifaceted approach. Initial treatment may involve fasting to rest the pancreas, IV fluids, and pain management. For long-term care, especially in chronic cases, dietary changes, enzyme supplements, and quitting alcohol are key strategies. In some cases, surgical interventions may be necessary to address complications or the underlying cause.
Prevention and Prognosis
- Maintaining a healthy lifestyle with a balanced diet and regular exercise
- Moderate alcohol consumption
- Regular medical check-ups to mitigate the risk factors
- Avoid toxins and chemical exposure that increase the risk of pancreatitis
With timely and appropriate management, the prognosis for acute pancreatitis is favorable. However, chronic pancreatitis may require ongoing treatment and lifestyle adjustments to manage symptoms and prevent further damage.
When to see a doctor?
It's important to know when to seek medical attention for pancreatitis.
- Severe abdominal pain that radiates to your back and doesn't improve within a day
- Pain accompanied by vomiting, fever, jaundice.
- Unusually fatty, oily, or smelly stools
- Changes in urination
- Persistent Nausea and Vomiting
- Unexplained weight loss